|
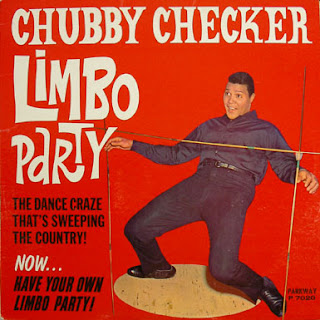
| Photo by M Clock |
But some facts that were contained in the article may.
As a direct result of Obesity on the rise, the burden of Diabetes Type 2 is staggering:
* At present, approximately 8.3% of the US population (25.8 million children and adults) have DM2, with approximately 7 million unaware currently of their disease state / diagnosis.
* An estimated 79 million adults have prediabetes.
* In 2010 alone, 1.9 million cases of DM2 were diagnosed in people aged 20 years and older.
* The cost of treating Diabetes and its associated complications was estimated to be $218 Billion in 2007, while Diabetes also contributed to more than 230,000 deaths.
And now to the MythBuster. As discussed earlier in this Blog in numerous places, the benefits of Bariatric Surgery, especially for diversionary procedures and VBG, start rapidly after surgery and are independent of weight loss. The weight loss does seem to reinforce the initial direct metabolic effect of the surgery, and enable a durable benefit for Diabetes and other metabolic conditions. .
LAGB (Laparoscopic Adjustable Gastric Banding) also aids in weight loss and Diabetes benefit, but through the dual effect of reduced dietary intake and weight loss over time. Even with medical (non-surgical) weight loss, the same is true of early blood sugar benefit in Diabetic patients via reduced dietary intake associated with "dieting" in most cases.
These facts about the severity and prevalence of the Diabetes epidemic are important to get us to act and be aggressive about treating Diabesity early through medical, and then possibly surgical means where indicated.
The facts about the metabolic benefits of the various surgical procedures also helps the differentiate among the different procedures. We keep this in mind as we discuss your patient's procedure of choice, but it its best for you to know, as the PCP, some of the basics about these procedures and their anticipated benefits, matching up the patient with their best option(s) when they first arrive to see us.
Of additional note, as you may have already noticed, patients of South or East Asian origin tend to have a much lower BMI with the same level of metabolic derangement than the typical patients that have metabolic syndrome / DM2 of European or African descent with a higher BMI.
Again, and in summary, once the specific metabolic benefits of surgery are more succinctly identified, they may be able to be harnessed pharmacologically without the need for surgery.
Maybe then it will be time to look for a new job... in sales and marketing?
Adapted form "Diabetes improvement after bariatric surgery is dependent on weight loss." Kaplan, Seeley, and Harris. Metabolic Applied Research Strategy, a supplement to Bariatric Times, Vol 9, No 9; Sept 2012.